Clinical Pharmacists: Reducing Patients Risk of Heart Attack or Stroke
The NHS is recognised worldwide for providing a high standard of healthcare to patients in the UK. It is constantly evolving to ensure this high standard is upheld.
As a result, roles of healthcare professionals are also developing and expanding. One of these roles includes clinical pharmacists.
This article explains how Clinical Pharmacists in GP practices help proactively manage patients’ health. They don’t just treat illnesses — they also help prevent them.
Understanding PCNs
Primary Care Networks (PCNs) started in 2019. They help GP practices work together and offer new services.
North Gosforth and Jesmond Lower Gosforth Primary Care Networks work collaboratively, under the banner of Gosforth and Jesmond Health, to provide additional expert services to patients at GP practice in the area.
Our PCN Team
Our team includes Clinical Pharmacists and Pharmacy Technicians. They are experts in using medicines to manage patients’ health.
Meet Our Clinical Pharmacy Team in North Gosforth:
- Ashling Kinsella, Lead Clinical Pharmacist and Project Lead
- Laura Larrieu, Clinical Pharmacist
- Suzanne Lenham, Clinical Pharmacist
- Naimah Muktadir, Clinical Pharmacist
- Mark Stafford, Clinical Pharmacist
- Chris Preece, Pharmacy Technician


What is Clinical Pharmacy?
Pharmacists are known as “medication experts”. They can have varied roles in community pharmacy shops, hospitals and GP practices.
Their role in GP practices includes prescribing and reviewing medication. They ensure patients medicines are safe, effective and used correctly.
Pharmacists are essential in meeting the ambitions of ‘The NHS long-term plan’ for disease prevention and optimising outcomes from medicines. The expansion of prescribing within the profession also helps support General Practice.
This project makes the next step and includes Pharmacists working in partnership with patients to help reduce the risk of Cardiovascular Disease (CVD) through discussion around lifestyle interventions and lipid-lowering therapy as a preventive treatment.
Cholesterol and Cardiovascular Disease
Cholesterol is a waxy, fat-like substance. You need the right amount of it in your body to be healthy.
Too much cholesterol – especially non-HDL or “bad” cholesterol – leads to build ups in arteries. This increases the risk of cardiovascular disease (CVD), like heart attacks or strokes.
CVD is a major cause of death and disability. It affects seven million in the UK and causes 1 in 4 premature deaths.
To try and reduce the risk, the NHS asks GP practices to make sure 70-95% of eligible patients take medication to lower their cholesterol. This is typically patients with Coronary Heart Disease, Chronic Kidney Disease, Peripheral Arterial Disease or have had a Stroke or Transient ischemic attack (TIA).
It’s an important preventative step, because lowering cholesterol can reduce the risk of CVD by up to 40%.
The first-line medicines in this group are called statins.
What Are Statins?
Statins are medicines that help lower non-HDL cholesterol. Patients simply take one tablet a day.
The dose depends on their cholesterol level and overall health. Some people may start on a low dose to see how they get pn, and monitoring and review with a Clinical Pharmacist, have the dose increased.
Like all medicines, statins may have mild side effects or interact with other medicines, so it’s important for Clinical Pharmacists to talk in detail with patients about the benefits and risks.
The Project in North Gosforth
The Pharmacy team reviewed patient data for the North Gosforth GP practices.
The NHS target is for 70-95% of eligible patients to be on lipid-lowering therapy.
All four GP practices were around the lower end of the target range. While this was a good starting point, the team knew more people could benefit.
But statins work behind the scenes — you don’t feel effects like with painkillers. So, the approach needed to be right.
The team needed to focus on prevention without alarming patients. It was crucial to help patients make informed decisions.
A mock-up of the messages patients received and an image of the Statins decision tool.
To help understand the risks and benefits of statins, NICE-approved patient decision aids were sent to patients so they could review the information available. This gave people time to think about their options.
Here’s how the project worked:
- The team found eligible patients (with the practice’s permission).
- Patients received a text with a link to the decision aid.
- The tool helped patients see how statins or similar therapies might help them.
- Patients could say no or ask to speak to the Clinical Pharmacy team.
- Lifestyle and medication options could be discussed in an appointment.
- If patients didn’t respond, the team would follow up with a call a month later.
The additional step of offering appointments to discuss the treatment options in detail is something Clinical Pharmacists are uniquely placed to deliver, and why this project stands aside from the everyday work of General Practice.
It combined proactive, preventative, personalised healthcare, shared decision-making and ensuring every contact with a patient makes a difference.
Patients benefited from in-depth discussions that explored the risks and benefits of statins or other lip-lowering therapies.
Not only could patients be introduced to the new and developing work the NHS is doing to reduce their risk of CVD, but the detailed and thorough clinical assessments the team were able to undertake meant patients would be getting the very best outcomes from any treatment they started.
Progress and Monitoring
The team also set aside special time slots to work on the project, track progress, and see the impact they were making.
This covered both continuing to contact patients to start the discussion about statins, but also full clinical assessments and monitoring.
This included:
- Clinical assessment, including lifestyle interventions
- Baseline blood tests
- Smoking status
- Alcohol consumption
- Exercise regime
- Height, weight and BMI
- Blood pressure
- Full lipid profile
- Liver transaminases
- Renal function
- Diabetes status;
- Creatine kinase (if the person has persistent generalized unexplained muscle pain);
- Thyroid-stimulating hormone (if the person has symptoms of an underactive or overactive thyroid).
- LFTs rechecked within 3 months and cholesterol profile around 3 months to check for effectiveness
For patients starting therapy, safety-netting was put in place around potential side-effects.
The Results
Over nine months, 320 additional patients started taking statins or another lipid-lowering therapy. That equates to one person every day making the informed decision to lower their risk of heart disease.
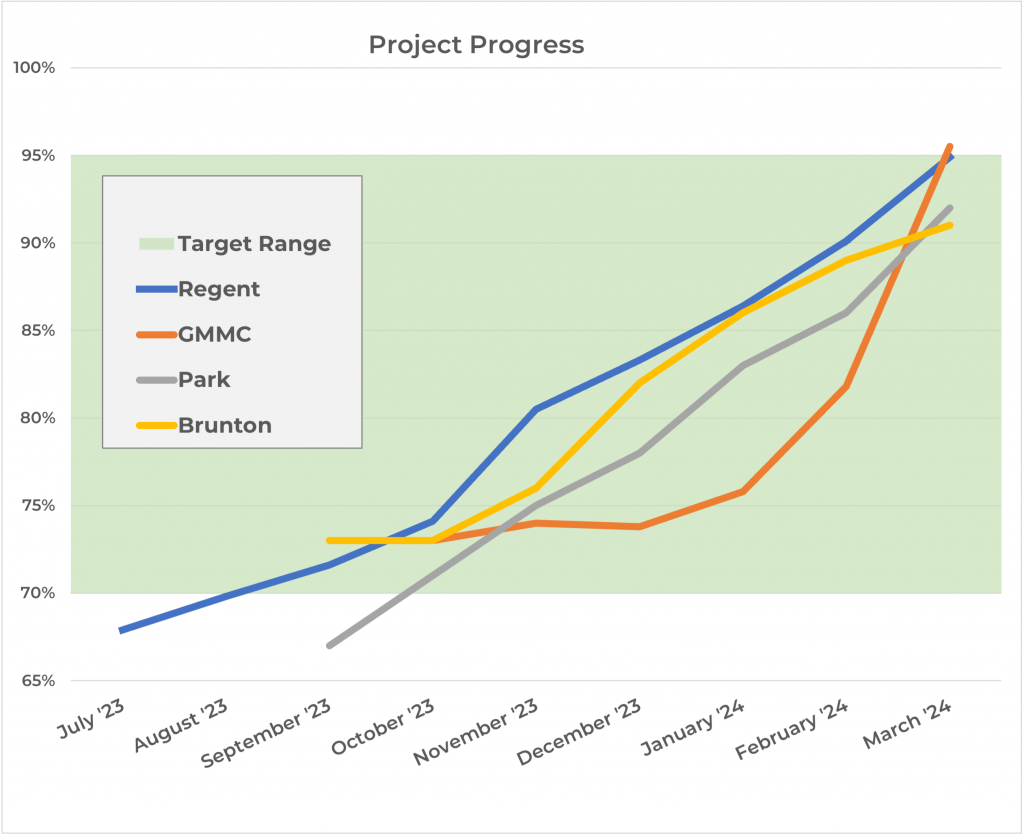
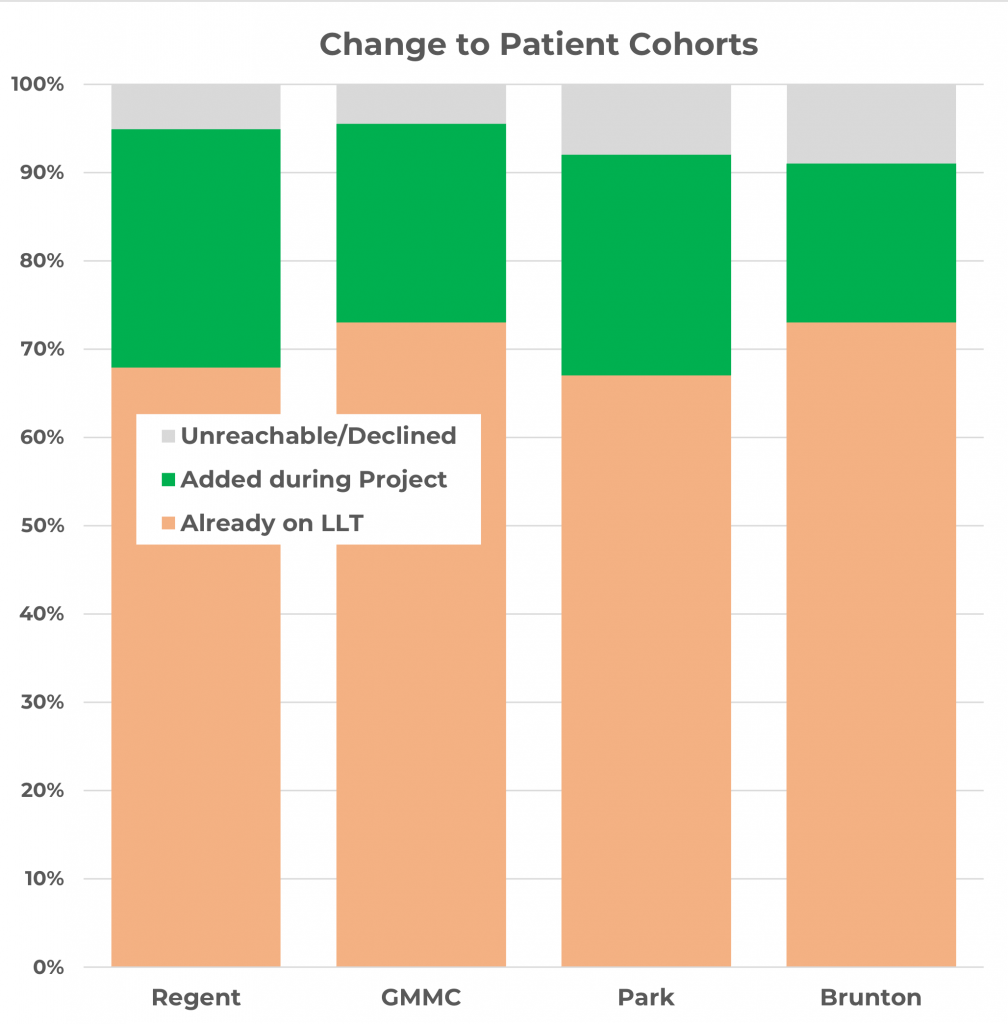
Now, all practices are at the top of the NHS target range. Only a few patients declined or have yet to respond.
The Benefits
The biggest benefit is the improved health of 320 patients. They are up to 40% less likely to have a heart attack, stroke, or develop vascular dementia.
The project also strengthened relationships between patients and the Clinical Pharmacy team. It introduced a new, proactive approach to healthcare.
Project lead Ashling Kinsella sums it up:
“This project introduced patients to the new NHS. Instead of just treating illness, they saw the value in preventing it – reducing their risk of cardiovascular disease.”
The team enjoyed the project. They liked watching long-term progress and knowing the work would benefit patients in the future.
