NHS Screening: How much does it help?
Last week we shared a news story on our website about how the NHS screening programme works.
It talked through the different things the NHS will screen for, when you might be invited and how the screening for each condition works.
You can read that story on our News page or by clicking or tapping the image below.

The gist of that story was that screening is a way to identify risk or very early signs of disease when it is easier to treat.
In this update, we will talk about how effective the screening programmes are – how many cancer cases and deaths they prevent.
You can read through the article for the full picture or skip to areas of interest with the buttons below.
Effectiveness
There are a few different ways to look at how effective health screening is.
The first is called morbidity – the number of confirmed cases of a certain disease or condition in the population.
The second is mortality – the number of deaths caused by that illness.
For a programme to be effective, it needs to make a difference in reducing both morbidity and mortality.
Of course, the screening programmes also need to cover the parts we talked about last week: the disease can be identified early; it is easier to treat when found early; and the process of screening is less harmful or invasive than the disease it’s looking for.
Last year, together with our neighbouring practices in Gosforth and Jesmond, we did a project to understand how people thought about cervical cancer and screening.
While previous campaigns had focussed on the ease of getting screened, patients told us that the high level of preventability was the strongest message.
So, following that through, let’s look at the number of cases and deaths of other conditions and how many could be prevented.
Video: Statistics
The video below runs through figures for four of the biggest screening programmes for adults: Breast, bowel and cervical cancer, and abdominal aortic aneurysm, or AAA.
In the sections that follow, we’ll explore these numbers.
Breast Cancer
If you are registered with your GP as a female, you’ll be offered breast screening, also called a mammogram, every three years. It begins at age 50 and continues to 74, as this is the highest-risk age range.
Here are the numbers:
- 1 in every 7 women will get breast cancer
- Nearly 56,000 cases are diagnosed every year in the UK
- 11,500 of those people will die from breast cancer – around 20%.
- That means every day in the UK, 32 people die from breast cancer
The next key figure to look at is preventability: 23% of all breast cancer cases can be prevented.
That means more than 2,600 lives could be saved through screening.
Despite this strong case for screening, the number of people booking appointments when invited has dropped.
In 2006, nearly three-quarters of people took up the offer of breast cancer screening. By 2021, that figure had dropped to 62.8% – barely 2 in every 3 females.
Bowel Cancer
Bowel cancer is the fourth most common cancer in both males and females. Risk of bowel cancer increases with age – 43% of cases are in people aged 75 or older – with men at slightly higher risk than women.
Test kits to use at home are sent every two years to people aged 60 to 74 (although a gradual expansion to include every in their 50s has now started).
The number of people taking the tests has increased in the last decade, but there are still some telling statistics:
- Around 43,000 cases diagnosed in the UK every year
- Nearly 17,000 deaths annual – a mortality rate of around 40%
- More than half – 53% of bowel cancer cases can be prevented
More than 8,000 lives could be saved every year through bowel cancer screening.
Back in 2010, only half of people eligible for a bowel cancer screening took the test. By 2021 this figure had got closer to 70%, but that still means nearly 1 in 3 test kits sent to people’s homes are never used.
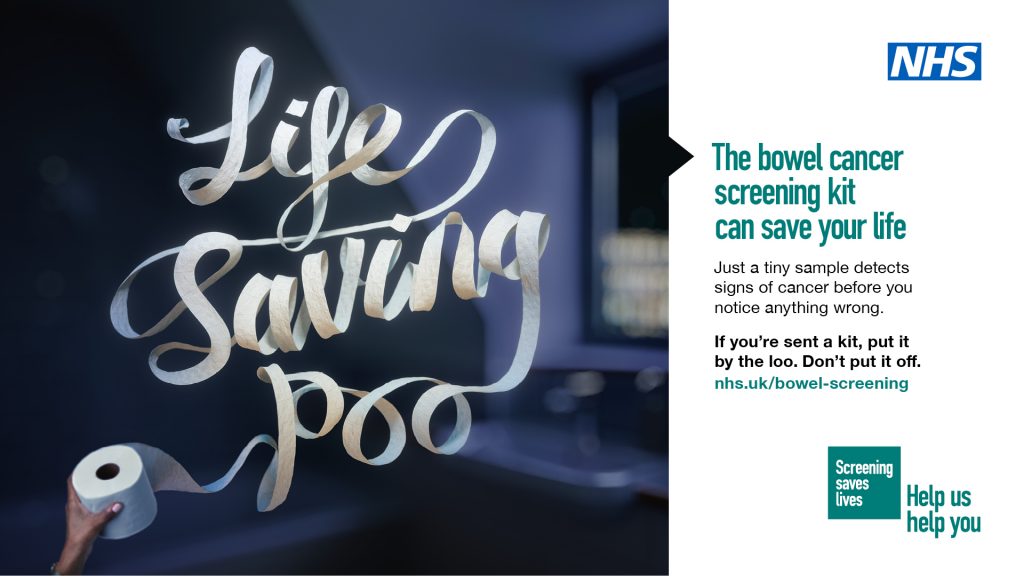
This high level of preventability comes from the test being able to spot early signs – namely, small amounts of blood in your poo – before you notice anything is wrong.
The NHS has recently launched a new campaign encouraging people to put their kit by the loo, not put it off. We shared the powerful campaign in March.
Cervical Cancer
We mentioned early the work we did with our neighbouring practices on cervical screening last year.
Our aim was to find out what people understood about the disease, their experiences of screening, both good and bad, and what we could do to encourage more people to attend.
Based on what people told us, we produced this video to answer some of your questions about changes to the test, why people who don’t have sex with men should still get tested, and what to expect at your appointment.
You can watch the video below.
The standout message was the preventability – 99.8%.
Here are the rest of the stats:
- 3,200 new cases yearly in the UK
- Around 850 deaths – more than 2 people every year
- 99.8% of cases are preventable
That statistic bears repeating. With regular screening, cervical cancer could be almost eliminated.
Cervical screening is offered to all women and people with a cervix from ages 25 to 64. The highest incidence is in people aged 30-34, so getting into the habit of regular screening is the best way to reduce your risk.
Abdominal Aortic Aneurysm (AAA)
AAA is slightly different to the cancers that are screened for. The screening looks for swelling in the aorta (the main blood vessel from your heart to your tummy).
Usually, there are no tell-tale symptoms. Often the first and only sign of an aneurysm or swelling in the aorta is when it ruptures.
80% of people who suffer a ruptured aorta die. AAA accounts for 6,000 deaths every year in the UK.
Older men are most at risk, and screening is offered in the year you turn 65.
If bulges are found, then, depending on the size, they can be monitored or operated on. Lifestyle changes can reduce risk and stop swellings from getting bigger.
All in all, screening reduces your risk of AAA by 50%.
Get screened
The choice to get screened for the conditions we’ve talked about is up to the individual. But there is a powerful evidence base that says screening is the best way to reduce your risk of serious illness or death.